Oocyte quality
Artificial Intelligence can now classify themWe are pioneers with this technology, unique in Asturias.
What do we talk about when we talk about oocyte quality?
Until now, only embryos were given a quality status, but oocytes were the forgotten ones. Now, thanks to the Artificial Intelligence that we have in our clinic, the oocytes can be classified and thus know in an objective way what their real quality is.
What is the purpose of knowing the quality of the oocytes?
Assessing the ovarian reserve allows us to anticipate how many eggs are left, but nothing tells us whether they are of good or poor quality. With Artificial Intelligence we can know if the quality of the oocytes may be the cause of a previous cycle with poor results, assess whether to vitrify more oocytes when we preserve fertility, or even assess whether it is time to move on to oocyte donation.
Know the quality of your oocytes
IVF or fertility preservation cycles
Applicable to past cycles
Artificial Intelligence to find out the quality of oocytes
At the ERGO Clinic we are pioneers in having the latest technology available at the service of assisted reproduction, and on this occasion we have done it again. Artificial Intelligence (AI) is coming to laboratories to help embryologists diagnose gametes.
It uses artificial intelligence algorithms based on Deep Learning, a model that is used to recognise patterns in large amounts of images that are invisible to the human eye. Our software has processed more than 60,000 oocyte (egg) images and their corresponding results to measure different fertilisation and blastulation rates in different types of patients.
Embryologists visualise oocytes on a daily basis and take into account different dysmorphisms (central granularity, vacuoles, perivitelline space, etc.) but it is still subjective and difficult to compare. However, this Artificial Intelligence scores the oocytes from 1 to 10, with 1 being the lowest quality and 10 being the highest quality.
The cases that have seen the most application have been:
- Fertility preservation. If, despite having a good number of vitrified eggs, they are of poor quality, it will be more difficult to achieve an evolutionary gestation with them in the future. Knowing this with the algorithm, it can be assessed whether it is advisable to repeat another cycle.
- Knowing the cause of infertility. There are several tests that can be performed on spermatozoa to determine their quality, but until now there was nothing as such for eggs. In this way it is possible to find out whether the eggs, despite their quantity and nuclear maturity, are of poor quality.
- Knowing the reason for a previous cycle with poor results. Some of the consequences of poor oocyte quality are poor quality, fragmented, blocked embryos, genetic alterations, implantation failure or repeated miscarriages. Knowing objectively the quality of these eggs can allow decisions to be made for the next cycle.
- VEvaluate a change to oocyte donation. This is the way to know if the suspicion of poor oocyte quality is a reality, and therefore to strengthen the idea of using donor eggs to achieve gestation.
Oocyte procurement
This phase is common to both in vitro fertilisation, fertility preservation and ROPA.
Between the 1st and 4th day of your period, you should come to the clinic for a gynecological check-up. Depending on the results of previous analytical tests, the ultrasound image we see and other personal parameters of your particular case, you will be prescribed the most appropriate medication.
With this medication, which is administered subcutaneously and you can inject it yourself in a very simple way in your belly, the ovaries are stimulated. It is a very simple process, and although on the day you are prescribed the medication we will explain in detail how to use it, you will always have our nursing team at your disposal to help you.
The stimulation lasts between 9 and 12 days, depending on each patient, during which several ultrasound and hormone tests are performed to see the response to the treatment and determine how to continue until the correct day of egg retrieval (also called ovarian puncture) is set.
Egg retrieval or follicular puncture
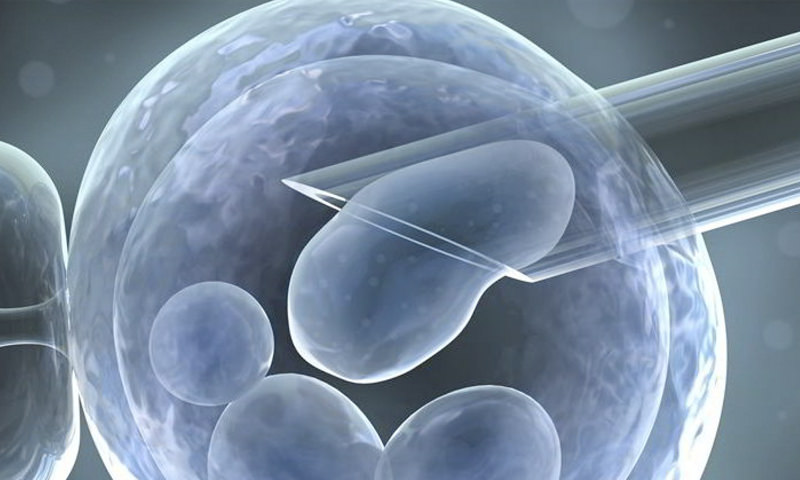
Once your follicles reach an adequate size, the ovarian puncture is scheduled. It is performed in the operating room, under anesthetic sedation, on an outpatient basis and without the need for hospitalization. During the 5-10 minute process, the follicular fluid is aspirated and the eggs are collected in the laboratory.
Everything is so fast that when you wake up, the eggs are already stored in the incubator in a specific culture medium and thus recovering the ideal physiological state.
Egg decumulation
After about two hours, the embryologists decumulate the oocytes (i.e. remove the cells that cover them) in order to assess their maturation status. Only those whose microscopic image is that of metaphase II (MII) will be eligible.
Egg imaging
The individually identified oocytes are placed under the micromanipulation microscope and the necessary images are captured and uploaded to the software.
Continuation of treatment
From that moment on, the initially planned treatment is continued.
If fertility preservation was to be performed, all mature eggs are vitrified on the spot.
In the case of in vitro fertilisation or ROPA, the corresponding sperm is prepared and ICSI is performed.
Applicable to pre-treatment
If you have done an IVF cycle or ROPA prior to the release of this technology, or you simply did the cycle in another centre. and you used the Geri Time-Lapse incubator system, we can also make that assessment.
We only need the first images of each of the oocytes that were captured in that incubator. And with this, we will have the quality assessment of each of the oocytes.
Need more information?
We are a team of more than 15 professionals specialized in assisted reproduction and women’s health. Do you have any doubts? We invite you to meet us, your first visit is totally FREE.